Phone
+91 7620308161
pinnacleendoscopy123@gmail.com
Location
KLLG st, No.99, Pku City, ID 28289
GI Sciences — Advanced Endoscopy & Digestive Care
Specialist-led diagnosis and treatment for oesophagus, stomach, intestine, liver, pancreas and bile duct conditions using advanced endoscopic techniques.

We provide comprehensive digestive evaluation and minimally invasive treatments under the care of a highly experienced gastroenterologist — ensuring accurate diagnosis, early detection and safe recovery.
BENEFITS
- Accurate diagnosis
- Minimally invasive treatment
- Early detection
- Faster recovery
PROCEDURES

Gastroscopy
(Upper GI Endoscopy)
What is it?
A camera-based examination of the oesophagus, stomach and duodenum.
Why/When you need it?
For acidity, reflux, ulcers, indigestion, bleeding or persistent upper GI symptoms.
What to expect during consultation?
Brief evaluation, symptom review, and preparation guidance for the procedure.
Treatment plan:
Endoscopic evaluation; biopsies or minor therapy if required.

Colonoscopy
What is it?
A detailed endoscopic examination of the large intestine.
Why/When you need it?
For rectal bleeding, altered bowel habits, polyps, inflammation or screening.
What to expect during consultation?
Assessment of symptoms and bowel-prep instructions.
Treatment plan:
Polyp removal, biopsy collection and targeted therapy during the procedure.

ERCP
(Endoscopic Retrograde Cholangiopancreatography)
What is it?
A combined endoscopy + X-ray imaging procedure for bile duct and pancreatic issues.
Why/When you need it?
For jaundice, stones, strictures, pancreatitis or abnormal scans.
What to expect during consultation?
Review of liver/pancreas reports and explanation of ERCP steps.
Treatment plan:
Stone removal, stent placement or therapeutic intervention.

Endoscopic Ultrasound (EUS)
What is it?
High-resolution internal imaging for pancreas, bile duct and GI lesions.
Why/When you need it?
For precise evaluation of tumors, cysts, stones or unexplained pain.
What to expect during consultation?
Discussion of symptoms and how EUS helps refine diagnosis.
Treatment plan:
Imaging with optional fine-needle aspiration if required.

Variceal Band Ligation / Glue Injection
What is it?
Endoscopic treatment to control bleeding from varices.
Why/When you need it?
For rectal bleeding, altered bowel habits, polyps, inflammation or screening.
What to expect during consultation?
Stability assessment, prior reports review and risk explanation.
Treatment plan:
Banding or glue therapy to prevent or stop active bleeding.

Polypectomy
What is it?
Removal of stomach or colon polyps during endoscopy.
Why/When you need it?
To reduce cancer risk or analyze suspicious growths.
What to expect during consultation?
Evaluation of symptoms and explanation of polyp removal safety.
Treatment plan:
Endoscopic excision of polyps with biopsy if needed.
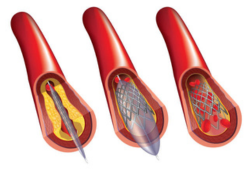
Metal Stent Placement (Esophageal / CBD / Enteral)
What is it?
Placement of a metallic stent to open narrowed or blocked passages.
Why/When you need it?
For difficulty swallowing, obstructive jaundice or intestinal blockage.
What to expect during consultation?
Diagnostic review and decision on type of stent required.
Treatment plan:
Endoscopic stent insertion tailored to the site of obstruction.
Argon Plasma Coagulation (APC)
What is it?
A non-contact thermal technique for bleeding control and tissue therapy.
Why/When you need it?
For GI bleeding, lesions or abnormal tissue requiring controlled therapy.
What to expect during consultation?
Evaluation of cause and discussion of APC benefits.
Treatment plan:
Targeted coagulation during endoscopy.

Capsule Endoscopy
What is it?
A swallowable camera that captures images of the small intestine.
Why/When you need it?
For unexplained anemia, bleeding, or suspected small-bowel disease.
What to expect during consultation?
Instructions on fasting and how the capsule process works.
Treatment plan:
Recording analysis and follow-up treatment based on findings.
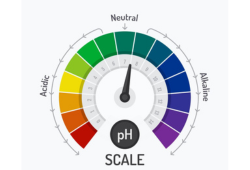
24-Hour pH Metry
What is it?
A test measuring acid reflux episodes over 24 hours.
Why/When you need it?
For persistent acidity or unclear GERD diagnosis.
What to expect during consultation?
Review of symptoms and explanation of probe placement.
Treatment plan:
Reflux management or medication adjustment based on results.

High-Resolution Manometry
What is it?
A test measuring the pressure and movement of the oesophagus.
Why/When you need it?
For swallowing difficulty, chest discomfort or motility disorders.
What to expect during consultation?
Explanation of the procedure and how results guide therapy.
Treatment plan:
Tailored treatment for motility issues such as achalasia.
FAQ
Sedation keeps the procedure comfortable.
Yes — most procedures are day-care.
Most are harmless but removed to prevent future risk.
Performed by trained specialists using advanced equipment.
